Chronic Obstructive Pulmonary Disease Prevalence and Mortality
- Introduction
Chronic obstructive pulmonary disease (COPD), sometimes referred to as chronic lung disease, is a disease that damages lung tissue or restricts airflow through the large and small airways leading to the air sacs in the lungs. Chronic bronchitis and emphysema are the most frequently occurring COPDs. Smoking is the most common risk factor for developing COPD, including cigarette, pipe, and cigar smoking (NHLBI, 2020). Other risk factors in the development and progression of COPD include asthma, exposure to air pollutants in the ambient air and workplace environment, genetic factors, and respiratory infections (CDC, 2011).
Secondhand smoke (SHS) may also increase the risk of developing COPD. The effect of chronic SHS exposure alone on pulmonary function in otherwise healthy adults is likely to be small. However, in combination with other exposures (e.g., prior smoking history, exposure to occupational irritants or ambient air pollutants), SHS exposure could contribute to chronic respiratory impairment (State of California, 2005). Reviews continue to call for additional research evidence to better evaluate the causal nature of the observed relationships between SHS and COPD (Eisner et al., 2010; HHS, 2014).
This indicator presents U.S. adult (age 18 and older) prevalence rates for chronic bronchitis and emphysema and U.S. adult (age 25 and older) death rates for all forms of COPD combined. Age-adjusted COPD prevalence data were compiled from 2002 to 2018 from the National Health Interview Survey (NHIS), conducted by the Centers for Disease Control and Prevention’s (CDC’s) National Center for Health Statistics (NCHS). The NHIS is the principal source of information on the health of the civilian non-institutionalized population of the U.S. and since 1960 has been one of the major data collection programs of NCHS. COPD prevalence is based on the number of adults who reported that they had ever been told by a doctor or other health practitioner that they had emphysema or if a health practitioner told them they had chronic bronchitis in the last 12 months.
Mortality data (age 25 and older) were compiled between 1979 and 2018 using the National Vital Statistics System (NVSS), maintained by NCHS. Because of the change of reporting requirements for race and ethnicity, data by demographic group (i.e., sex, race, ethnicity, and age group) were compiled for the years 1999 to 2018, when data are available to compare more races and ethnicities. The NVSS registers virtually all deaths and births nationwide, with data coverage from 1933 to 2018. The NVSS collects data from 57 vital registration jurisdictions, including all 50 states, the District of Columbia, New York City, and five U.S. territories (NCHS, 2020). Data were queried and compared separately for years 1979-1998 and those 1999 onward because the NVSS uses different codes to specify causes of death for these two time periods: the International Classification of Diseases 9th Revision (ICD-9) codes for 1979-1998 and the International Classification of Diseases 10th Revision (ICD-10 codes) beginning in 1999.
- What the Data Show
COPD Prevalence
Exhibits 1 and 2 present the age-adjusted prevalence of chronic bronchitis and emphysema from 2002 to 2018, respectively. The reported total prevalence of chronic bronchitis in U.S. adults over the age of 18 years has generally decreased during this time period, ranging from a high of 44 cases per 1,000 (2002) to a low of 33 cases per 1,000 in 2017. The reported prevalence of emphysema in U.S. adults during the same time period fluctuated, with the highest rate of 21 cases per 1,000 in 2009 and the lowest in 2017 (12 cases per 1,000).
Exhibits 1 and 2 also display age-adjusted chronic bronchitis and emphysema prevalence in U.S. adults, respectively, by race, ethnicity, and sex; age-specific prevalence is also presented. For the 17 years shown for chronic bronchitis, differences in rates by race were observed where whites have the highest prevalence in five years, American Indians/Alaska Natives have the highest prevalence in nine years, and Blacks or African Americans have the highest prevalence in three years. Asians have the lowest prevalence of chronic bronchitis in all 17 years reported (Exhibit 1). For 13 of the 17 years reported, emphysema prevalence is highest among white adults. American Indians/Alaska Natives have the highest prevalence for four of the 17 years reported. Asians consistently have the lowest prevalence of emphysema except in 2006, when the prevalence for Asians is above that of Blacks or African Americans and in 2017 and 2018, when the prevalence for Asians is above that of American Indians/Alaska Natives (Exhibit 2). Prevalence of both bronchitis and emphysema rises with age, with the highest rates generally seen among those 65 and older.
The Hispanic or Latino population had a consistently lower prevalence of chronic bronchitis (Exhibit 1) and emphysema (Exhibit 2) than the non-Hispanic or Latino population from 2002 to 2018, the period for which these data are available. For example, in 2018, prevalence in Hispanics or Latinos was lower than non-Hispanics or Latinos for chronic bronchitis (27 compared to 36 cases per 1,000, respectively) and emphysema (10 compared to 14 cases per 1,000, respectively). Prevalence also differs by sex. In 2018, females had about 2.0 times the reported prevalence of chronic bronchitis compared to males (45 versus 23 cases per 1,000, respectively), a consistently observed difference between 2002 and 2018 (Exhibit 1). In contrast, the prevalence rates for emphysema were consistently higher in males than in females from 2002 to 2018, with the exception of 2011, when the prevalence rates were the same (19 cases per 1,000). The difference between male and female emphysema rates varied by as much as 12 cases per 1,000 in 2006 to as little as 1 case per 1,000 in 2008, 2014, and 2017 (Exhibit 2).
COPD Mortality
In 2018, chronic lower respiratory disease, primarily COPD, was the fourth leading cause of mortality in the United States (General Mortality indicator) (CDC, 2020a,b). Specifically, in 2018, COPD accounted for 155,987 (5.6 percent) of all deaths among adults aged 25 years and older (CDC, 2020b). Exhibit 3 shows that the age-adjusted death rate for COPD as a whole has increased over time, with national rates ranging from 37.4 per 100,000 in 1979 to 61.4 per 100,000 in 1998. From 1999 to 2018, rates held steadier, ranging from a high of 67.6 per 100,000 in 1999 to a low of 59.9 per 100,000 in 2018.
Age-adjusted death rates for emphysema (range of 9.5-10.9 per 100,000 for 1979-1998, and 2.8-10.0 per 100,000 for 1999-2018) and chronic bronchitis (range of 1.4-2.6 per 100,000 for 1979-1998 and 0.1-0.3 per 100,000 for 1999-2018) appear to be slowly declining or steady. It is noteworthy that in 2018 approximately 78 percent of all COPD mortality is of an unspecified nature and not attributed to a specific COPD subgroup such as emphysema or chronic bronchitis (CDC, 2020b; data not shown).
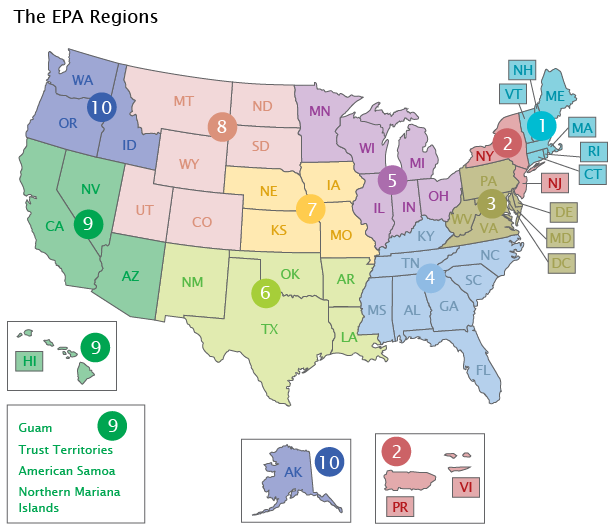
Exhibit 3 presents the overall COPD death rates in the U.S. and the 10 EPA Regions for 1979-1998 and 1999-2018. The age-adjusted COPD death rates increased in each of the 10 Regions between 1979 and 1998. The rates ranged from 32.2 (Region 2) to 45.8 (Region 8) per 100,000 in 1979 and 48.8 (Region 2) to 70.6 (Region 8) per 100,000 in 1998. A decline in COPD death rates occurred in each of the 10 EPA Regions between 1999 and 2018.
Exhibit 4 presents age-adjusted COPD death rates from 1999 to 2018 among U.S. adults aged 25 years and older by sex, race, ethnicity, and age group. As shown, COPD age-adjusted death rates have been declining for males over time, with a rate of 88.6 per 100,000 in 1999 compared to 66.3 per 100,000 in 2018. For females, the rates are lower than males and have been relatively stable between 1999 and 2018 (55.2 and 55.3 per 100,000, respectively). Rates declined among the races shown, with the highest age-adjusted death rates consistently observed among whites (ranging from 71.5 per 100,000 in 2008 to 64.4 per 100,000 in 2018) and the lowest rates observed among Asians or Pacific Islanders (ranging from 26.4 per 100,000 in 1999 to 16.6 per 100,000 in 2018). Rates also declined by ethnicity, with 33.3 per 100,000 in 1999 compared to 25.0 per 100,000 in 2018 among the Hispanic or Latino population. Rates for those not Hispanic or Latino are higher, but still declined from 1999 (69.2 per 100,000) to 2018 (63.2 per 100,000). COPD death rates also vary by age, with higher rates observed among older age groups. For example, the 2018 rates were 0.5 per 100,000 for those aged 25-44 years, 21.8 per 100,000 for those aged 45-64 years, and 267.1 per 100,000 for those aged 65 years and older.
- Limitations
- Prevalence data presented in the NHIS are based on self-reported responses to specific questions pertaining to COPD-related illnesses, and are subject to the biases associated with self-reported data. Self-reported data can underestimate the disease prevalence being measured if, for whatever reason, the respondent is not fully aware of his/her condition.
- COPD death rates are based on underlying cause of death as entered on a death certificate by a physician. Some individuals may have had competing causes of death. “When more than one cause or condition is entered by the physician, the underlying cause is determined by the sequence of conditions on the certificate, provisions of the ICD [International Classification of Diseases], and associated selection rules and modifications” (CDC, 2020c). Consequently, some misclassification of reported mortality might occur in individuals with competing causes of death, as well as the possible underreporting of COPD as the cause of death.
- The International Classification of Diseases 9th Revision (ICD-9) codes were used to specify underlying cause of death for years 1979-1998. Beginning in 1999, cause of death is specified with the International Classification of Diseases 10th Revision (ICD-10) codes. The two revisions differ substantially, and to prevent confusion about the significance of any specific disease code, data queries are separate.
- Data Sources
COPD prevalence data were obtained from annual reports and standalone tables published by NCHS (NCHS, 2004, 2005, 2006a,b, 2007, 2009a,b, 2010, 2012a,b, 2014, 2015a,b, 2016, 2018a,b, 2019), which summarize health statistics compiled from the NHIS (https://www.cdc.gov/nchs/nhis/nhis_series.htm). Mortality statistics for 1999 to 2018 were obtained from CDC’s Underlying Cause of Death database, accessed through CDC's Wide-ranging Online Data for Epidemiologic Research (WONDER) Online Database (CDC, 2020b) (https://wonder.cdc.gov/ucd-icd10.html). Mortality statistics for 1979-1998 in Exhibit 3 came from the CDC WONDER Compressed Mortality database (CDC, 2016) (https://wonder.cdc.gov/mortSQL.html). EPA Regional mortality statistics were generated by combining and age-adjusting state-by-state totals for each EPA Region using data from CDC WONDER.